Prostatitis isa purely male disease. It is one of the most common lesions of the genitourinary system and occurs in approximately 80% of men, with 4 of them occurring before the age of 40 years.
The disease is not an isolated process: itexposes nearby organs to traumatization and also poisons the entire body.
How does prostatitis develop?
The essence of the process is inflammation of the prostate or prostate gland.
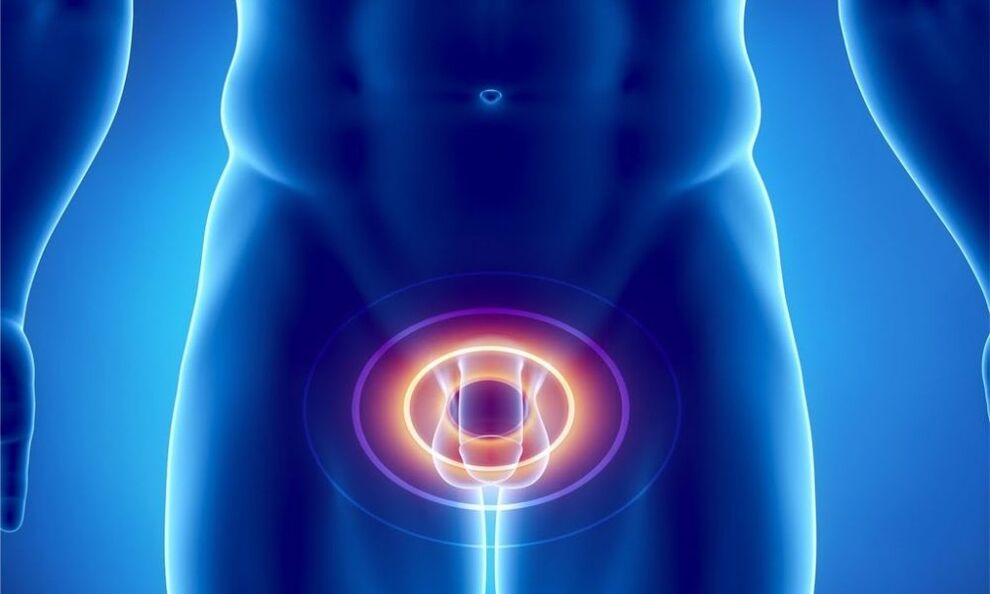
The prostate is located in the pelvis, adjacent to the bottom of the bladder. This is an unpaired organ that looks like a chestnut. The urethra passes through it. Behind the gland is the rectum, and in front of it is the pubis.
The prostate gland is a fairly elastic organ, because its basis is made up of muscle fibers and glandular cells. It consists of 2 lobes, which are connected by an isthmus. It is the main source of problems associated with urination. Densifying and increasing in size with age, the isthmus puts pressure on the urethra, disrupting the process of urine excretion.
Prostateperforms such functions for the body:
| Function | The essence |
|---|---|
| Secretory | Produces a secretion that is part of sperm. It dilutes it, sets the required pH level, and increases sperm motility. |
| Motor | The muscle fibers of the gland form the urinary sphincter, which helps to hold back urine. |
| Barrier | Contains a zinc-peptide complex, lysozyme, cellular immunity factors, spermine, which prevent the development of infection in an ascending manner. |
Prostatitis develops when an inflammatory process starts in the gland. At the same time, it increases in size, squeezing the urinary canal. This causes difficulty urinating.
In addition, the enlarged prostate "intrudes" into the bladder, squeezing it. Because of this, the evacuation of urine from it is disrupted, it stagnates, causing inflammation now in the bladder. Long-term stagnation of urinary fluid in its "reservoir" leads to intoxication of the entire body with metabolic products in its composition.
Contributing Factors
The main reason for the development of prostatitis isinfection. This can be staphylococcus, enterococcus, Klebsiella, Pseudomonas aeruginosa and Escherichia coli, Proteus. Most often, prostatitis isa consequence of sexually transmitted diseases: syphilis or gonorrhea, chlamydia, trichomoniasis.
Less commonly, the cause of the disease isinfectious processes of other systems: flu, tuberculosis, tonsillitis and others. Bacteria and viruses enter the prostate through lymph and blood flow, as well as through sexual contact. Quite often, pathogenic flora is introduced into the gland via the ascending route from the urethra or descending from the bladder with infected urine.
Other factorsthat provoke inflammation of the gland include:
- circulatory disorders in the pelvis. This can be caused by a sedentary lifestyle, excess weight, and pelvic injuries. A special risk group is represented by drivers who are constantly in a sitting position and experience vibration and pressure on the perineal area. Reduced blood circulation in the pelvis causes congestion and lack of oxygen in the prostate gland, which also provokes the development of infection,
- hypothermia,
- hormonal imbalance,
- problems with passing urine,
- irregular sexual activity – too "violent" sex life, abstinence, interruption of sexual intercourse,
- chronic constipation,
- inflammation of the rectum,
- decreased immunity, as a result of which the body becomes susceptible to infectious agents.
There is an opinion that the risk of developing the disease increases with regular use of alcohol and drugs.
Typification and symptoms of the disease
In the modern world, the division of prostatitis into types is carried out according to the classification of the US National Institutes of Health in 1995. Itbased on clinical data, as well as the presence of leukocytes and pathogenic flora in seminal fluid, prostate secretion and urine:
- Acute bacterial prostatitis.
- Chronic bacterial prostatitis.
- CPPS – chronic pelvic pain syndrome or chronic non-bacterial prostatitis.
- Asymptomatic prostatitis.
Acute prostatitisis infectious in nature. There are several stages:
- catarrhalAccompanied by frequent and painful urination. The pain radiates to the sacrum and perineum,
- follicular.The intensity of the pain increases. It also appears during defecation. Urination becomes difficult - urine comes out in a thin stream or drops. Hyperthermia up to 38°,
- parenchymatous.Characterized by acute urinary retention and problems with bowel movements. Severe pain in the perineum, lower back and above the pubis. Body temperature rises to 38-40°. Intoxication of the body develops, the symptoms of which are general weakness, nausea, and increased heart rate.
During a digital examination by a urologist, an enlarged, dense prostate gland is palpated, hot and painful to the touch. A large number of leukocytes and bacteria are detected in the urine.

Chronic prostatitiscan develop as a consequence of an acute disease or as a separate disease. The diagnosis is made if the process lasts 3 months or more.
Chronic prostatitis manifests itself in 3 main syndromes:
- painful.Interestingly, the prostate itself does not contain pain receptors. Pain appears when the inflammatory process seizes the nerve fibers of the small pelvis, in which there are quite a lot of them. It is of a different nature. It can be insignificant or sharp and strong, disturbing even at night, subsiding and resuming again. It is localized in the sacrum, scrotum, lower back and perineum.
- dysuric.The urge to urinate becomes more frequent. It becomes sluggish, and there is a feeling of a heavy, not completely emptied bladder. Then the process may improve due to a compensatory increase in the muscles of the bladder, but soon resumes again. Discharge appears from the urethra during bowel movements.
- sexual disorders– an increase in nocturnal erections or a decrease in it, blurred orgasm, pain during ejaculation and its acceleration. Worsening sexual disorders, which ultimately lead to impotence. There is a concept of psychogenic dyspotence, when a man convinces himself that in his condition, violations in the intimate sphere are inevitable. And they are actually developing. With the development of sexual dysfunction, a man’s mood also changes: he becomes irritable and depressed.
Often the chronic form of prostatitis becomes a manifestation of hidden sexually transmitted infections.
Diagnosis of CPPSis placed if clinical manifestations of prostatitis are present, but pathogens of the disease are not detected in biological fluids (urine, ejaculate and prostate secretions). Leukocytes are determined at the same time.
The main criterion for diagnosis is pain that does not subside within 3 months.
Chronic pelvic pain syndrome is divided into 2 categories: inflammatory and non-inflammatory.
Inflammatory CPPSdetermined when a large number of leukocytes are found in biological fluids. Bacteria are not detected.
Non-inflammatory CPPScharacterized by the absence of leukocytes and pathogenic flora in biological fluids.
In both cases, symptoms of prostatitis persist.
Asymptomatic formThe disease is characterized by the absence of signs of prostate inflammation. It is discovered accidentally during histology of prostate tissue if the patient has been prescribed a prostate biopsy. A similar procedure is prescribed, for example, when PSA levels increase.
The disease, regardless of its type (except for the asymptomatic form), manifests itself, first of all, urinary disorders:
- pain when passing urine,
- weak stream or dribble of urine,
- feeling of the bladder not being completely empty.
If such symptoms appear, do not delay visiting a urologist. This will help stop the process at its first stage.
How to recognize the disease
The main criterion for making a diagnosis is the clinical picture and complaints of the patient.
But to finally confirm it,it is necessary to undergo a series of tests and examinations:
- Examination by a urologist.The doctor must conduct a rectal examination of the prostate. It is passed with a finger through the rectum. It is advisable to have a bowel movement before the examination. Using manipulation, the shape and size of the gland, as well as its consistency, are determined. The procedure helps to determine the presence of tumors and inflammation in the prostate. Digital examination allows you to collect prostate secretions.
- Analysis of urine.Two portions are examined: urine collected at the beginning of urination, and urine collected at the end of the process. 1 serving indicates the condition of the urethra, 2 – the kidneys and bladder. The presence of leukocytes in the urine above normal (15 per field of view) indicates inflammation.
- After collecting urine, a prostate massage is performed, as a result of which its secretion is obtained.If there is too little of it and it is not released from the urethra, but remains on its walls, urine is collected after the massage. It is as informative as the prostatic discharge itself. Leukocytes are also determined here (there should not be more than 10 of them), and, additionally, lecithin grains and amyloid bodies. If the first analysis of gland secretion did not show any abnormalities, this does not mean the absence of a process. Prostate juice may be too viscous and clog the lumen of the ducts of the affected glands. Then the secretory secretion will be produced by healthy glandular cells. Therefore, it is necessary to pass such an analysis several times. Cultures of urine and prostate secretions are also performed to identify the causative agent of the disease and determine sensitivity to antibiotics.
- General blood analysis.
- Analysis for the presence of sexually transmitted diseases.
- Ultrasound of the kidneys, bladder, TRUS,which allows you to thoroughly assess the condition of the prostate,
- Uroflowmetry.It is used to evaluate the rate and time of urine excretion. It is carried out with a special apparatus consisting of sensors and a container. All the patient needs to do is urinate into it in the usual way.
- Blood PSA– prostate specific antigen. It is an indicator of the presence of tumor formations in the prostate gland - adenoma or cancer,
- Prostate biopsy.It is carried out if the presence of cancer is suspected.
It is necessary to take a spermogram, which will help confirm or refute infertility.
Therapy of acute and chronic prostatitis
Acute prostatitis without complications is usually treated on an outpatient basis. Hospitalization is indicated for severe intoxication or the development of complications.
Treatment of acute prostatitisstart with antibiotics. If the condition is sharply disturbed, they are administered without waiting for the results of the analysis. They use groups of antibacterial drugs that are able to penetrate deep into the tissues of the prostate gland. They act on those types of bacteria that most often cause inflammation in it. These antibiotics include fluoroquinolones.

Upon receipt of testsantibiotic therapy may be adjusted differently. It all depends on the causative agent of the disease and its sensitivity to the drug. Therapy is also changed if no effect is observed after 2 days.
In case of acute inflammation of the prostate gland, the administration of painkillers, as well as non-steroidal anti-inflammatory drugs, is indicated. In addition to oral medications, suppositories are also used, which also have an analgesic and anti-inflammatory effect: based on prostate extract, suppositories with propolis.
In case of severe intoxicationcarry out detoxification therapy. To do this, use a glucose solution.
Prescribed drugs that improve blood circulation in the prostate. They ensure the drainage of lymph from the gland, relieve swelling, and promote the elimination of toxins.
In case of acute prostatitis, it is forbidden to massage the gland, as this can provoke the development of sepsis.
Treatment of chronic prostatitis depends on the stage of the disease.
In the acute form, antibiotics are used. In the remission stage, therapy is aimed at maintaining the normal functioning of the gland:
- Drugs that normalize organ microcirculation.
- Anti-inflammatory drugs.
- It is important to maintain the body's immune function, which decreases under the influence of courses of antibiotics. For this, patients are prescribed immunostimulants.
- For sexual dysfunction, it is possible to prescribe antidepressants and sedatives.
- Prostate massage.
- Physiotherapy:
- laser,
- ultrasound,
- rectal electrophoresis,
- transrectal microwave hyperthermia.
- Physiotherapy.

Physiotherapy for prostatitis helps increase the tone of the pelvic floor muscles and reduce pain.
Prostate massage: purpose and technique
Finger massage of the prostate has several purposes.
It is used as a diagnosis, to obtain gland secretions, and also as a method of treating chronic prostatitis.
MostA common method for this procedure is transrectal. In this case, the patient is placed on his right side with his knees bent. The doctor inserts the index finger into the anus, moving it along the rectum. Then a massage is performed: gentle stroking of each lobe of the gland around it and along the ducts. At the end of the procedure, the furrow between the lobes is kneaded to release secretory fluid.
It is necessary to focus on the patient’s sensations: there should be no pain during manipulation. The procedure lasts 1 minute, the full course is 15 sessions.
An indicator of a high-quality massage is the release of a few drops of gland secretion.
Such manipulation, first of all,increases blood circulation in the prostate. This accelerates tissue repair and improves the passage of medications, eliminates congestion and relieves inflammation.
Massage helps strengthen the muscles of the gland and perineum. The procedure allows you to remove stagnant seminal fluid from the organ, due to which the prostate is cleansed of bacteria and toxins. Compression of the urethra is eliminated and urination is improved. Massage increases potency by increasing the circulation of seminal fluid.
In addition to the transrectal method, there is an instillation method and bougie massage.
Instillation methodbegins with the introduction of a medicinal solution through the urethra. Then it is clamped and the prostate is massaged using the finger method. In this case, the healing solution penetrates the gland, enhancing the effect of the procedure. At the end, the urethra is unclenched, it is recommended to wait a while with urination. The drug is reintroduced into the urethra.
Bougie massageperformed through the urethra using bougies - special instruments for dilation and examination of tubular organs. The patient is in the right lateral position. The bougie is inserted into the urethra and held with one hand. With the second hand, stroke and press on the penis from top to bottom. The duration of the procedure is 1 minute, after which the drugs are administered intraurethrally. This massage is supported by antibiotic therapy.
Finger massage of the prostate– medical manipulation, which is performed by a specialist according to clear indications.
An option for self-massage is possible: to do this, rhythmically tense and relax the muscles around the anus. This procedure will be invisible to others and will help strengthen the gland.
Like any manipulation,Prostate massage has its contraindications:
- acute inflammation of the prostate,
- cancer or adenoma of the gland,
- haemorrhoids,
- stones, cystic formations in the prostate organ.
A professionally performed procedure will help restore the structure of the prostate and its function, and stimulation of sensitive points will eliminate sexual dysfunction.
Prostatitis and traditional medicine
Along with medications, traditional methods will also help to cope with inflammation of the prostate. Combining these 2 types of treatment, you will speed up the healing process and get rid of unpleasant sensations.
There are many home recipes that help in the fight against prostatitis. Here are some of them:
- Grind 500 grams of peeled raw pumpkin seeds through a meat grinder and mix with 200 grams of honey. Make small balls from the resulting mass. Consume before meals 2 times a day, slowly, chewing and dissolving thoroughly. Pumpkin seeds contain a large amount of zinc, which is essential for men's health.
- blueberries have an anti-inflammatory effect. By eating 200 grams of this berry a day, you will support your men's health,
- Parsley, first of all, became famous as a culinary spice. But besides this, it also contains a lot of useful substances, including those that the male body needs. Take parsley juice 1 tbsp. l. 3 times a day 30 minutes before meals. This will help relieve inflammation and improve sex life,
- take the green peel of the chestnuts along with the thorns, chop them and pour boiling water over them. Use as tea
- Grind 300 grams of onion to a paste-like consistency, add 100 grams of honey, 600 ml of dry wine. Keep for 1 week in a dark and cool place, stir occasionally. Strain. Use 2 tbsp. l. 3 times a day before meals. Effective in the treatment of chronic prostatitis.
Some will help speed up recoveryphysical exercise. They stimulate blood circulation in the pelvic area and, accordingly, in the prostate.
- Deep squats below knee level. The optimal number of times is 100. Perform 3 times a week. If you cannot do such a number at once, perform squats in several approaches with breaks.
- Scissors. Sit on the floor with your hands on the floor behind you. Stretch your legs in front of you, lift them off the floor. Cross them over each other. The movements resemble the work of scissors.
- Lying on your back, bend your knees and bring them to your chest. Wrap your arms around them. Hold the pose for up to 20 minutes.
- Regular walking is also a great way to relieve congestion.
You cansupplement this complex with other exercises, which activate and warm up the muscles.
Teenage prostatitis
It’s hard to believe, but prostatitis, which was considered the province of middle and old age, is now significantly younger and is found even among teenagers. It negatively affects the condition of the entire body, as well as the reproductive ability of young people.

That's whyit is important to understand the reasonsthat lead to teenage prostatitis:
- early sexual activity and sexual illiteracy.Unprotected sexual intercourse contributes to the flourishing of sexually transmitted infections, which can cause bacterial inflammation of the prostate,
- hypothermia– a contributing factor in the development of prostatitis. Temperature imbalance reduces immunity and exposes the body to infectious attack,
- fashion trends– wearing clothes and underwear that are too tight disrupts blood circulation in the pelvis and leads to stagnation in this area,
- sedentary lifestyle– work on the computer of modern youth replaces sports, walks and other active pastimes,
- excessive sexual activityliterally depletes the gland. Its functions are reduced, and the small amount of secretion released and the deterioration of its quality make it more susceptible to infections.
Prostatitis manifests itself in young people in different ways. Some are concerned about obvious symptoms: hyperthermia, severe pain in the groin with irradiation to neighboring organs and when urinating. For others, symptoms occur in a mild form. General weakness, decreased activity, low-grade fever, and urethral discharge appear.
VeryIt is important not to ignore the signs of the disease, but to start treatment on time. The neglected pathological process will leave its mark on the condition of the organ and the lives of young men.
Preventive actions
It is better to prevent any disease than to treat it. Measures to prevent prostatitis are quite simple, and they are not difficult to follow.
- First of all,reconsider your daily routine. If you have a sedentary job, be sure to introduce five-minute sports exercises into your routine. Stretch your body, move more. This is necessary to make the blood "run" faster through the vessels. At the same time, avoid excessive physical activity, which exhausts the body.
- Stop smoking. Tobacco smoke spasms blood vessels and impairs blood circulation, reducing the supply of oxygen to the prostate gland. Limit your intake of alcoholic beverages.
- Avoid hypothermia and nervous tension.
- It is worth eating marinated dishes, as well as spices and pickles, and hot sauces in doses.
- Regularity of sexual activity and adequacy of sexual intercourse should be observed.
Untreated prostatitis threatens a number of complications: transition to a chronic form, development of infertility, spread of the process to the kidneys and bladder. More serious consequences include adenoma and prostate cancer. It is possible that purulent foci – abscesses – may appear in the gland and become septic.
As you can see, the disease is quite insidious. And, despite the delicacy of the issue, you should not delay her treatment. Block the process in the early stages of its development: only in this case will you preserve your health and virility.























